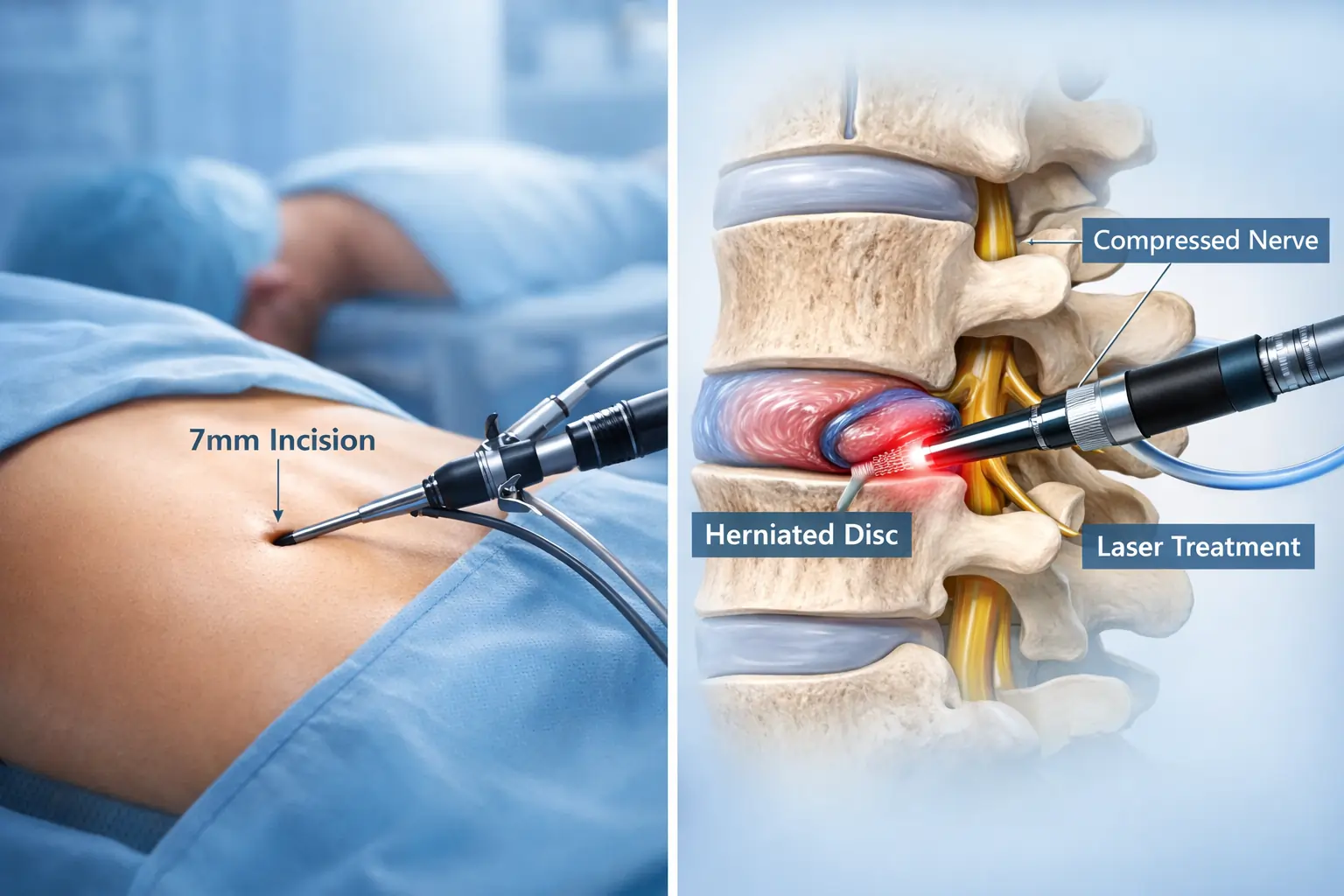
What is PELD? Percutaneous Endoscopic Lumbar Discectomy (PELD) is a minimally invasive spine surgery that treats slip disc through a tiny incision using an endoscope, avoiding traditional open surgery's extensive muscle cutting and bone removal.
Why Your Back Pain Might Need More Than Just Rest
I've seen thousands of patients walk into my clinic over the past 25 years, and I can tell you this: back pain changes lives. Not always in dramatic ways, but in small, frustrating ones. You stop playing with your kids. You avoid that morning walk. You cancel plans because sitting in a car feels impossible.
Most people try everything before considering surgery. Pain medications. Physiotherapy. Those epidural injections everyone talks about. And honestly? That's exactly what you should do. About 80-90% of slip disc cases get better without surgery.
But what about the other 10-20%? What happens when six weeks turn into six months, and the pain down your leg makes you want to scream?
This is where we need to talk about surgery. Not the kind your grandfather had, with big incisions and months of recovery. I'm talking about PELD, a procedure that's changing everything we thought we knew about treating slip discs.
Here's What Most Doctors Won't Tell You About Traditional Spine Surgery
Let me be honest with you. Traditional open discectomy works. It's been the gold standard for decades, and surgeons have performed millions of these procedures successfully.
But here's the part nobody likes to discuss: traditional spine surgery cuts through healthy tissue to reach the problem.
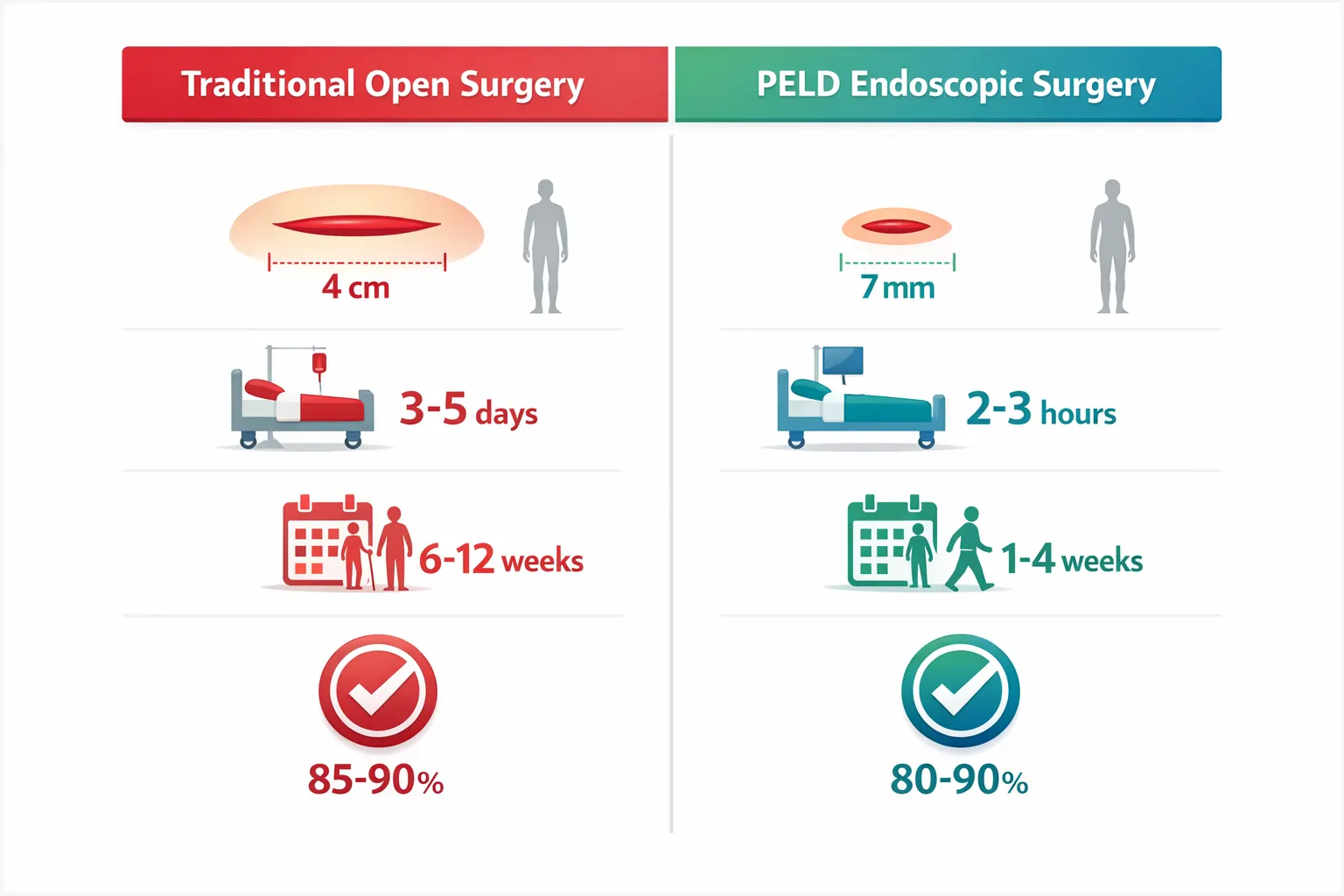
Think about it this way. Your disc herniation might be the size of a peanut. But to remove it through open surgery, we need to make a 3-4 cm incision, pull apart muscles, sometimes shave off bone, and create quite a bit of damage getting to that tiny problem.
You'll spend 3-5 days in the hospital. You'll need general anesthesia. Recovery takes 6-12 weeks. And about 8-12% of patients develop complications.
Is there a better way? That's exactly what German surgeons asked themselves back in 1987.
The German Innovation That Changed Spine Surgery Forever
Here's something fascinating: German orthopedic surgeons pioneered PELD because they wanted precision. They asked a simple question: "Why make a big hole when a small one works just fine?"
The answer was revolutionary. They developed a technique using an endoscope (basically a tiny camera on a flexible tube) that could reach herniated discs through an incision smaller than your fingernail.
At Germanten Hospital, we've brought this German precision technology to Hyderabad. Why? Because having trained in Germany myself, I saw firsthand how this approach transforms patient outcomes.
What Actually Happens During PELD Surgery (The Part Nobody Explains)
Most websites give you vague descriptions. Let me walk you through what actually happens, step by step.
Before Surgery Starts: You'll lie on your stomach or side. We use local anesthesia with light sedation. Yes, you read that right. Most patients don't need to be fully asleep. You can actually talk to me during the procedure. This matters tremendously for elderly patients or those with heart conditions who can't safely undergo general anesthesia.
The Two Approaches Nobody Tells You About:
This is critical. PELD isn't one-size-fits-all. We use two different approaches depending on where your disc herniated:
Transforaminal Approach (Through the Side): When your disc bulges sideways, I access it through the natural opening between your vertebrae called the foramen. Think of it as entering through a doorway that already exists. No bone cutting needed. This works beautifully for L4-L5 and L5-S1 level herniations (the most common locations).
Interlaminar Approach (From the Back): For central disc herniations or when the fragment has migrated, I approach from between the laminae bones in your back. This gives me more working space and better access to remove fragments that have traveled.
Which approach do you need? That's determined by your MRI. This is why bringing your imaging to consultation matters so much.
During the Procedure: I make a 7-8mm incision. Using live X-ray guidance (fluoroscopy), I insert a small tube to create a working channel. The endoscope goes through this tube, giving me a crystal-clear, magnified view of your spine's internal structures.
I can see the herniated disc fragment, the compressed nerve, everything. Using tiny instruments (forceps, shavers, radiofrequency probes), I carefully remove only the problem tissue. Not healthy disc material. Just the herniation pressing on your nerve.
The whole thing takes 30-60 minutes.
One stitch closes the incision. That's it.
The Success Rate Truth That'll Surprise You
Here's what the research actually shows: PELD has an 80-90% success rate. That's comparable to traditional open surgery.
But success depends heavily on two factors most patients don't know about:
Factor 1: Patient Selection Not everyone is suitable for PELD. I'll be brutally honest here because your outcome matters more than our surgical numbers.
You're an ideal candidate if:
- You're under 60 years old (outcomes are statistically better)
- Your herniation is contained, meaning the disc fragment hasn't completely separated and migrated far
- You have single-level disc disease
- Conservative treatment failed after 6-12 weeks
- Your leg pain is worse than your back pain
- Your MRI shows a lateral or posterolateral herniation
You're NOT a good candidate if:
- Your disc has sequestrated (completely broken off)
- You have severe spinal instability
- You need extensive decompression for stenosis
- You have cauda equina syndrome (this needs emergency open surgery)
- Your disc is heavily calcified
- You have active infection
This selectivity matters. Some surgeons push PELD for everyone. That's wrong. Proper patient selection is why our success rates stay high.
Factor 2: Surgeon Experience
Here's the uncomfortable truth: PELD has a steep learning curve. Medical studies show that surgeons performing their first 20-30 cases have significantly higher complication rates.
When you're choosing a surgeon, ask these questions:
- How many PELD procedures have you performed?
- What's your complication rate?
- How often do you need to convert to open surgery mid-procedure?
- Do you perform both approaches (transforaminal and interlaminar)?
At Germanten Hospital, being one of the best orthopedic hospitals in Hyderabad, we've performed hundreds of these procedures. Experience matters when you're working through a space the width of a pencil.
What Nobody Tells You About Recovery (The Real Timeline)
Websites promise "same-day discharge" and "quick recovery." That's true, but incomplete. Let me give you the honest week-by-week breakdown:
Day 1: You'll walk within 2-3 hours of surgery. Yes, really. Most patients go home the same day or next morning. Pain level? Usually 3-4 out of 10. Way less than before surgery.
Week 1: Walking is encouraged. What's off-limits? Lifting anything heavier than 2 kilograms, bending forward, twisting your spine. You might experience some leg pain. This is normal. Your nerve is healing and sometimes protests a bit.
Weeks 2-4: If you have a desk job, you can return to work. Driving is okay if you're pain-free. Light household chores are fine. This is when physiotherapy starts.
Weeks 4-6: Most people return to their jobs. You can swim, walk longer distances, resume most normal activities. Heavy lifting and contact sports? Still off the table.
Months 2-3: Full recovery. Sports clearance happens case-by-case. Your disc continues healing for up to two years.
The Caveat: About 6-10% of patients experience recurrence. Usually within two years. Risk factors? Heavy lifting, obesity, smoking, genetics. This is why lifestyle modification isn't optional. It's essential.
The Hidden Advantages Medical Websites Don't Mention
Everyone talks about smaller scars and faster recovery. But PELD offers benefits that go way deeper:
Advantage 1: Preserved Spinal Mechanics Traditional surgery cuts facet joints and muscles that stabilize your spine. PELD leaves everything intact. This prevents "failed back surgery syndrome," a devastating condition where surgery creates more problems than it solves.
Advantage 2: Local Anesthesia Capability Remember how I mentioned you can be awake? This is huge for:
- Diabetic patients (better blood sugar control)
- Cardiac patients (no stress on heart)
- Elderly patients (lower risk profile)
- Anyone afraid of general anesthesia
Plus, if you can communicate during surgery, you can immediately tell me if something feels wrong. That's an extra safety layer.
Advantage 3: Inflammatory Response Reduction Research shows PELD causes 65% less systemic inflammation than open surgery. Less inflammation means faster healing, lower infection risk (under 1% vs 2-3% for open surgery), and better long-term outcomes.
Advantage 4: Future Options Remain Open If you develop another disc herniation years later (a different level), PELD can be repeated. Traditional surgery often makes future minimally invasive options impossible because of scar tissue.
Let's Talk Money (The Part Everyone Wonders About)
In India, PELD costs between ₹4-8 lakhs ($5,200-10,000). Traditional open surgery? ₹6-12 lakhs.
But here's the real calculation:
- Fewer hospital days
- Faster return to work
- No prolonged physiotherapy
- Lower complication costs
The true savings come from getting your life back weeks earlier.
Most insurance companies and TPAs cover PELD. At Germanten Hospital, we handle cashless claims for empaneled organizations. Always verify pre-authorization before surgery.
The Risks Nobody Wants to Discuss (But You Deserve to Know)
Any surgery carries risks. Here's the honest breakdown:
Overall complication rate: 4.89% (compared to 8-12% for open surgery)
What can go wrong:
Dural Tear (0.1-4.9%): The protective covering of your spinal cord can tear. Usually, this heals on its own. Rarely needs surgical repair.
Nerve Root Injury (2-3%): Usually temporary irritation. Permanent injury happens in less than 0.5% of cases. This is almost always related to surgical learning curve.
Incomplete Decompression: Sometimes, a fragment remains. About 3.66% of patients need revision surgery.
Recurrence (6.3%): Your disc can herniate again at the same level. Usually happens within two years. The good news? It can often be re-treated with PELD.
Compare this to traditional surgery, and PELD comes out ahead on safety.
When PELD is NOT the Answer (And What to Do Instead)
Not every back pain needs surgery. Not every surgery needs to be PELD.
Try Conservative Treatment First:
- Physical therapy focusing on core strengthening
- NSAIDs (with stomach protection)
- Lifestyle modifications
- Weight loss if applicable
Give this 6-12 weeks. It works for 80-90% of patients.
Consider Interventional Procedures: Transforaminal epidural steroid injections provide 70-80% pain relief for 3-12 months. They're not just "pain killers." They reduce inflammation around the nerve, helping it heal.
When Surgery Becomes Necessary: If conservative treatment fails, progressive neurological weakness develops, or your quality of life is severely impacted, then we talk surgery. But PELD versus traditional surgery? That depends on your specific anatomy and herniation pattern.
The Questions My Patients Actually Ask
"Will I be awake during surgery?" Usually, yes, with conscious sedation and local anesthesia. You won't feel pain, just some pressure. If you prefer being fully asleep, general anesthesia is available.
"Can I fly home afterward?" Most international patients can fly 24-48 hours post-surgery. Wear compression stockings and walk every hour during the flight.
"What if it doesn't work?" About 3-4% of cases need conversion to open surgery. If PELD doesn't provide adequate relief, microdiscectomy remains an option. No bridges are burned.
"How long does relief last?" Studies show 90% of patients maintain relief at five years. But this requires lifestyle changes: core strengthening, weight management, proper ergonomics.
What You Should Do Right Now
If you've been suffering from leg pain, numbness, or weakness for more than six weeks, and conservative treatment isn't working, it's time for evaluation.
Bring your MRI to consultation. As one of the top orthopedic doctors in Hyderabad with specialized training from Germany, I'll tell you honestly whether PELD is right for you or if another approach makes more sense.
Not everyone needs surgery. Not everyone needs PELD. But if you're the right candidate, this procedure can give you your life back with minimal disruption.
We're living in an era where spine surgery doesn't have to mean six weeks in bed. German engineering brought precision to orthopedics. We've brought that precision to Hyderabad at Germanten Hospital, recognized as one of the best ortho hospitals in Hyderabad.
Your Next Step Toward Pain-Free Living
The decision to have surgery (any surgery) should never be taken lightly. But living in chronic pain, giving up activities you love, watching life pass you by while you're stuck on the couch? That's not living either.
PELD isn't magic. It won't fix everything. But for the right patient with the right herniation pattern, treated by an experienced surgeon, it's as close to magic as spine surgery gets.
Here's what I want you to remember:
- PELD success depends on proper patient selection
- Surgeon experience matters tremendously
- Recovery is faster, but lifestyle changes are essential
- Not everyone is a candidate, and that's okay
- Traditional surgery remains excellent for cases not suitable for PELD
One question to ask yourself: If you could reduce your recovery from 12 weeks to 3 weeks, preserve your spinal stability, and achieve the same pain relief with a fraction of the tissue damage, wouldn't you at least want to know if you're a candidate?
Schedule a consultation. Bring your MRI. Let's have an honest conversation about your options. No pressure. No sales pitch. Just straight answers from someone who's spent 25 years figuring out the best ways to fix spines.
Because you deserve to know all your options. And you deserve to get better.
Ready to explore if PELD is right for you? Contact Germanten Hospital to schedule a consultation with Dr. Mir Jawad Zar Khan, one of the best orthopedic surgeons in Hyderabad, trained in advanced spine surgery techniques in Germany with over 10,000 successful surgeries.