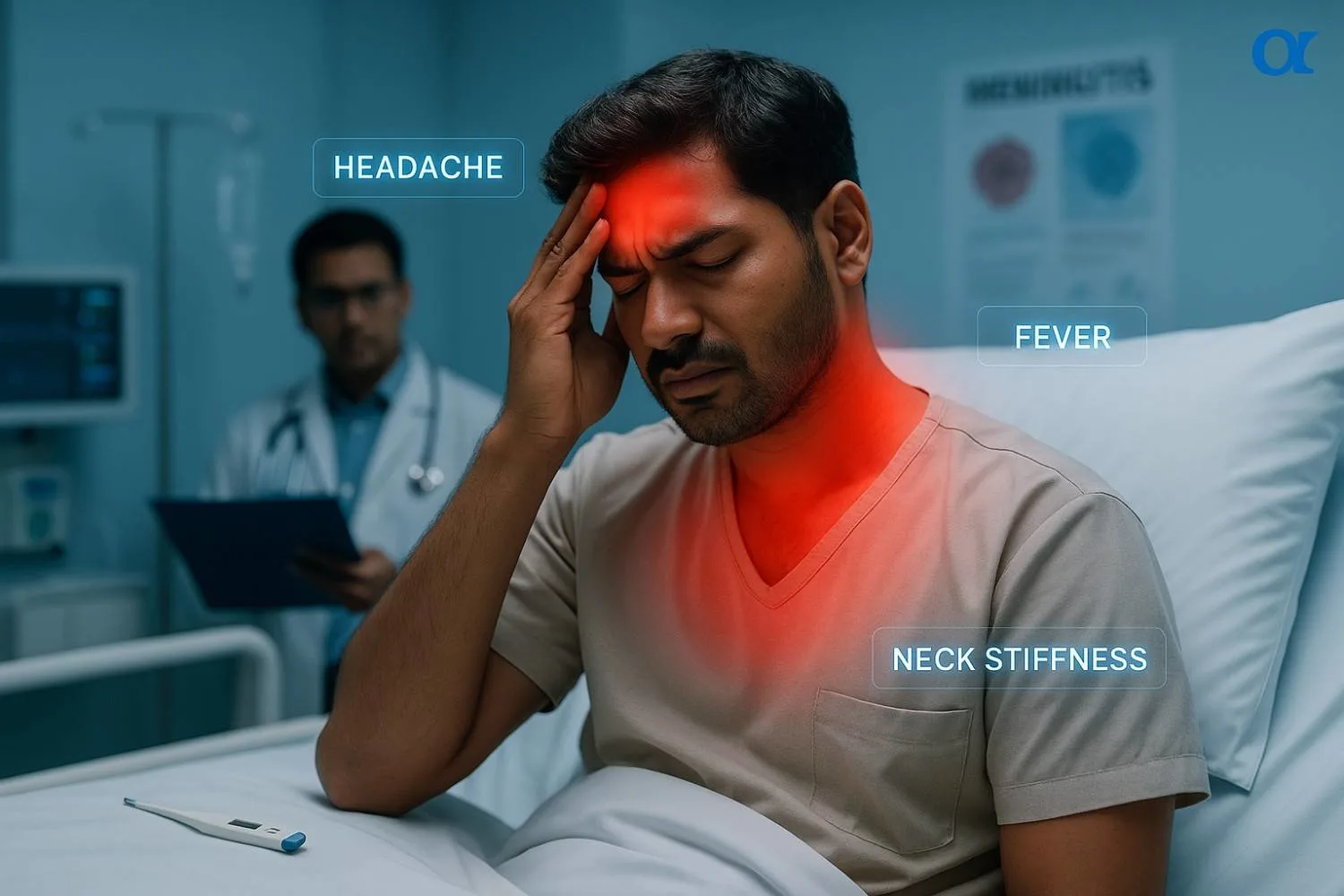
It often starts with familiar feelings. A headache that won't quit, a sudden fever that makes you shiver, and a strange stiffness in your neck. For many, these are just signs of the common flu. But in rare cases, this classic trio of symptoms can be the first warning of something far more serious: meningitis.
Meningitis is an inflammation of the protective membranes that cover the brain and spinal cord. Usually caused by a viral or bacterial infection, it requires urgent medical attention because, without swift treatment, it can lead to severe, long-term complications or even become life-threatening.
Understanding the difference between a common illness and the early signs of meningitis is not just helpful—it can be critical. This guide will walk you through the key symptoms, explain who is most at risk, and provide a clear action plan so you know exactly what to do if you suspect meningitis.
The Classic Trio: Decoding the Main Symptoms
While meningitis has many potential symptoms, medical professionals are always on high alert for three key indicators. The presence of this "classic triad" is a strong signal that immediate medical evaluation is needed.
The Unrelenting Headache
This isn't your average tension headache. A meningitis headache is typically described as severe and persistent. It often feels different from other headaches you've had. The pain might radiate down your back or be so intense that it's difficult to concentrate or even tolerate light.
The Sudden High Fever
Unlike a cold that develops over a few days, the fever associated with meningitis often comes on suddenly and can be very high. You might experience chills as your body temperature spikes. This rapid onset is a crucial clue that you're dealing with more than a minor bug.
The Telltale Stiff Neck
This is perhaps the most distinctive symptom. A stiff neck from meningitis isn't just about muscle soreness. It's a painful stiffness that makes it difficult to lower your chin to your chest. In children, they may hold their neck still or cry when it's moved. This stiffness is caused by the inflammation of the meninges surrounding your spinal cord.
Beyond the Basics: Other Critical Symptoms to Watch For
While the classic trio is a major warning, meningitis can present with a wider range of symptoms that can develop over several hours or a few days. It's vital to be aware of these other signs, as they provide a more complete picture of the illness.
General Symptoms in Adults and Older Children
In addition to the three main ones, be on the lookout for:
- Nausea and Vomiting
- Sensitivity to Light (Photophobia): A strong dislike of bright lights is a very common symptom. You might find yourself needing to be in a dark room to feel comfortable.
- Confusion or Altered Mental State: Difficulty concentrating, feeling disoriented, or extreme sleepiness are serious signs.
- Seizures: The inflammation can trigger convulsions or fits.
- The Meningitis Rash: In some cases, particularly with meningococcal meningitis (a type of bacterial meningitis), a distinctive rash may appear. It often starts as small, red pinpricks and can quickly spread, turning into red or purple blotches that look like bruises.
The Glass Test: A Critical Action You Can Take If you see a rash, perform the "glass test." Push the side of a clear glass firmly against the spots. A normal rash will fade under pressure. A meningitis rash will not fade. This is a sign of sepsis (blood poisoning) and is a medical emergency. You should call for an ambulance immediately. It's important to note that this rash can be more difficult to see on brown or black skin, so check paler areas like the palms of the hands, soles of the feet, or the inside of the eyelids.
Meningitis in Babies and Infants: The Signs Are Different and More Subtle
Recognizing meningitis in babies and young children is especially challenging because they can't tell you what's wrong. The symptoms are often different from those in adults and can be mistaken for other common childhood illnesses. Parents must trust their instincts.
What to Look For in Your Baby
If your baby is unwell, watch for these signs in any combination:
- Fever: Though some babies under 3 months may not have a fever.
- Refusing to Feed: A sudden lack of interest in eating or a weak suck during feeding.
- Extreme Irritability: Constant, high-pitched crying that can't be soothed.
- Drowsiness or Sluggishness: Being unusually sleepy, difficult to wake, or slow to respond.
- A Bulging Fontanelle: The delicate spot on the top of a baby's head may feel firm or bulge outwards.
- Stiffness or Floppiness: Their body may seem stiff, sometimes with an arched back, or they may be unusually floppy and unresponsive.
- Vomiting
Seizures, sometimes brought on by a fever, can be one of the first signs of meningitis in infants and young children. If you see these symptoms, especially if your child seems to be getting sicker quickly, seek medical help immediately.
Why You Must Act Fast: Bacterial vs. Viral Meningitis
Not all meningitis is the same. The cause of the infection—whether it's a virus or bacteria—dramatically changes the outlook and treatment.
- Viral meningitis is the most common type and is usually less severe. Most people recover fully on their own with rest and supportive care.
- Bacterial meningitis is much rarer but is a life-threatening medical emergency. It can progress incredibly quickly and, without immediate antibiotic treatment, can lead to permanent disability or death.
Because the initial symptoms can be identical, doctors will always treat suspected meningitis as bacterial until it is proven otherwise.
Comparison: Bacterial vs. Viral Meningitis
To make it simpler, here's a table comparing the symptoms of a common backache with serious red flags.
| Feature | Bacterial Meningitis | Viral Meningitis |
|---|---|---|
| Cause | Caused by bacteria like Neisseria meningitidis or Streptococcus pneumoniae. | Caused by viruses, most commonly enteroviruses, but also herpes, mumps, or measles viruses. |
| Severity | Very serious. A medical emergency that can be fatal or cause permanent disability. | Usually less severe. Most people make a full recovery, though it can still make you very unwell. |
| Contagiousness | Contagious. Spread through respiratory droplets (coughing, sneezing, kissing). | Contagious. Can be spread through coughing, sneezing, or poor hygiene (fecal contamination). |
| Treatment | Requires immediate hospitalization and intravenous (IV) antibiotics. | No specific treatment for most viruses. Managed at home with rest, fluids, and pain relief. |
| Long-Term Effects | High risk. Can include hearing loss, brain damage, seizures, and limb loss. | Rare. Most people recover fully, though fatigue and headaches can persist for some time. |
Why 'Waiting it Out' is the Most Dangerous Thing You Can Do
With a common cold or flu, the standard advice is often to rest and wait. This is the absolute wrong approach for suspected meningitis. Bacterial meningitis can progress from early symptoms to a life-or-death situation in a matter of hours. A study from the Karolinska Institutet found that one in three children who survive bacterial meningitis live with permanent neurological disabilities. The World Health Organization (WHO) estimates that 1 in 6 people who get bacterial meningitis will die. Delayed treatment is the single biggest factor that increases the risk of these devastating outcomes.
Who Is Most at Risk?
While anyone can get meningitis, some groups have a higher risk of infection. Key risk factors include:
- Age: Viral meningitis is most common in children under 5, while bacterial meningitis is common in those under 20, especially infants under one year old.
- Living in Group Settings: The bacteria that cause meningitis can spread fast in crowded environments like college dorms, military bases, and childcare facilities.
- A Weakened Immune System: People with conditions like HIV or cancer, or those taking medications that suppress the immune system, are more vulnerable.
- Not Being Vaccinated: Risk rises significantly for anyone who has not completed the instructed childhood or adult vaccination schedules.
Getting a Diagnosis: What to Expect at the Hospital
If a doctor suspects meningitis, they will act quickly to confirm the diagnosis. The process typically involves several steps to rule out other conditions and identify the exact cause.
- Physical Exam: The doctor will inspect for the classic signs, including fever, neck stiffness, and any skin rashes.
- Blood Tests: A blood specimen will be taken to check for bacteria or viruses and signs of inflammation in the body.
- Imaging Scans: A CT scan of the brain may be done to check for swelling or other problems that could make a lumbar puncture unsafe.
- Lumbar Puncture (Spinal Tap): This is the most important test for diagnosing meningitis. A thin needle is inserted into the lower back to collect a small sample of cerebrospinal fluid (CSF), the fluid that covers the brain and spinal cord. This fluid is then tested in a lab to see if there is an infection and, crucially, to determine if it is caused by bacteria or a virus. This test provides the definitive answers needed to guide treatment.
The Path Forward: Treatment, Recovery, and Prevention
Treatment for meningitis depends entirely on the cause. If bacterial meningitis is even a remote possibility, doctors will start treatment immediately, often before all test results are back.
Treatment and Recovery
- Bacterial Meningitis: Treatment involves high-dose intravenous (IV) antibiotics administered in a hospital. Corticosteroids may also be given to reduce swelling and lower the risk of complications. Recovery can take a long time, and some people are left with permanent after-effects.
- Viral Meningitis: Since antibiotics don't work on viruses, treatment focuses on managing symptoms. This usually includes bed rest, plenty of fluids, and over-the-counter pain relievers. Most people heal fully within 7 to 10 days.
Life After Meningitis: The Potential Long-Term Effects
Surviving bacterial meningitis is a major victory, but for many, the battle isn't over. The WHO reports that one in five survivors may experience long-lasting after-effects. These can include:
- Hearing loss (the most common after-effect)
- Memory and concentration problems
- Recurrent seizures (epilepsy)
- Movement and balance issues
- Vision loss
- Limb loss due to sepsis
Your Best Defence: Prevention Through Vaccination
The best way to protect yourself and your family from several types of bacterial meningitis is through vaccination. The main vaccines used in India and around the world are:
- Meningococcal Conjugate (MenACWY) Vaccine: Protects against four common types of meningococcal bacteria (A, C, W, and Y). It is routinely recommended for preteens and teens.
- Serogroup B Meningococcal (MenB) Vaccine: Protects against a fifth type of meningococcal bacteria (B). This is often recommended for teens and young adults, especially those living in dorms.
- Other Childhood Vaccines: Such as the pneumococcal and Hib vaccines, also protect against bacteria that can cause meningitis.
Your Action Plan: What to Do if You Suspect Meningitis
If you or someone you know has symptoms that could be meningitis, every second counts. Do not hesitate.
- Trust Your Instincts: You know your body and your child best. Do not wait for a rash to appear or for all the symptoms to be present. If something feels seriously wrong, act on it.
- Get Medical Help Immediately: Call for an ambulance or go to the nearest hospital emergency department right away. Explain that you are concerned about meningitis.
- Be Ready to Share Information: When you speak to the doctor, be prepared to tell them about the symptoms, when they started, and your vaccination history.
A headache, fever, and stiff neck can be alarming, and it's right to be cautious. While they are often signs of a less serious illness, they are also the calling card of meningitis. By knowing the full range of symptoms—especially the subtle signs in babies and the emergency signal of a non-fading rash—you are empowered to act quickly and decisively. When it comes to meningitis, that speed can make all the difference.