Receiving an MRI report can feel like trying to read a foreign language. Words like "disc bulge," "herniation," "protrusion," and "degeneration" can sound alarming, often creating more anxiety than clarity. If you're holding a report right now, filled with technical terms and feeling a wave of concern, take a deep breath. You've come to the right place.
At Germanten Hospitals, we believe that an empowered patient is a healthier patient. Our philosophy, built on a foundation of German technological precision and decades of surgical expertise, starts with one simple thing: clear, honest communication. This guide is designed to do just that. We will walk you through your MRI report, demystify the jargon, and provide the crucial context you need to understand what these findings really mean for your health.
Think of us as your expert guide on this journey. We're here to turn confusion into confidence and fear into understanding, helping you take the first step toward a precise diagnosis and a life free from pain.
First, A Quick Anatomy Lesson: Understanding Your Spine's Shock Absorbers
Before we can decode the report, let's quickly understand the part of your spine in question: the intervertebral disc. Your spine is made up of a series of bones called vertebrae, stacked one on top of the other. Between each of these bones lies a disc, which acts as a shock absorber and a flexible pivot point, allowing you to bend and twist.
The "Jelly Donut" of Your Spine: The Intervertebral Disc
The easiest way to understand a disc's structure is to think of a jelly donut. This simple analogy is used by spine specialists around the world because it's incredibly accurate. The disc has two main parts:
- The Annulus Fibrosus: This is the tough, fibrous outer ring of the disc, much like the doughy part of the donut. It's made of multiple, crisscrossing layers of strong cartilage, engineered to be incredibly resilient and to contain the soft center under pressure.
- The Nucleus Pulposus: This is the soft, gel-like center, similar to the jelly filling. It has a very high water content, which gives it the ability to absorb and distribute the immense forces your spine endures every day.
The health of your entire spine depends on this simple but brilliant design: a tough outer wall containing a soft, shock-absorbing core. Nearly all disc problems arise when this structure is compromised.
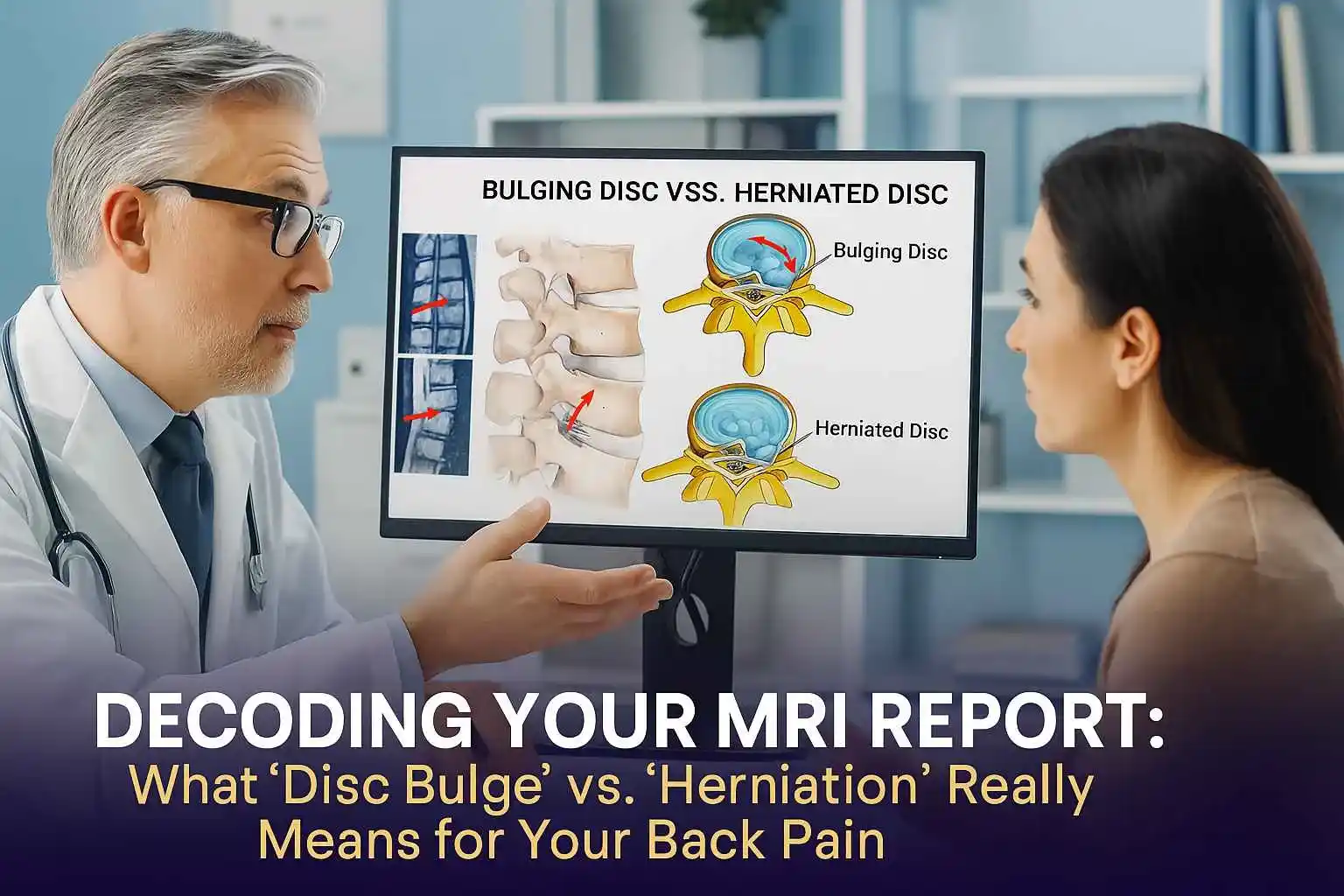
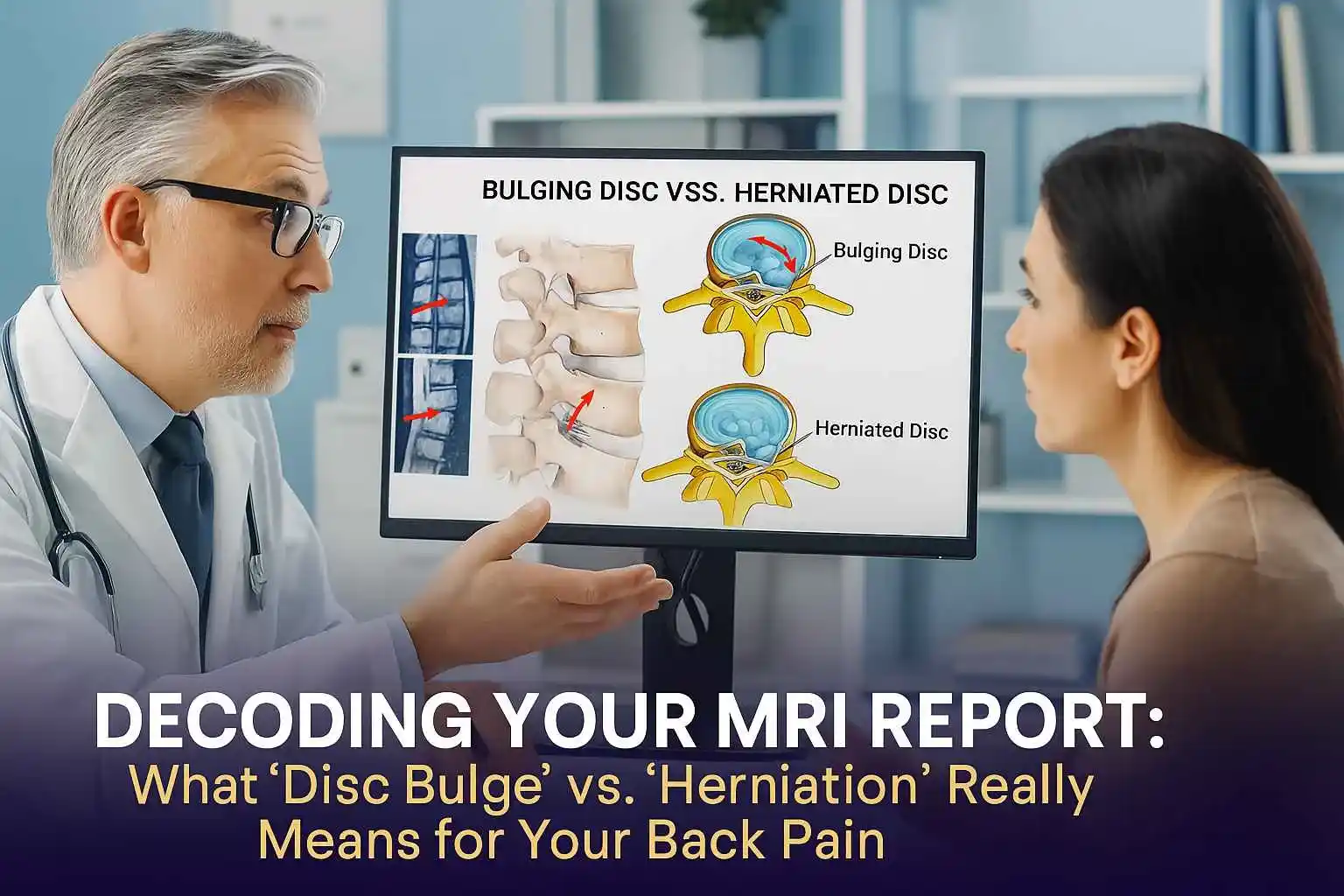
Disc Bulge vs. Disc Herniation: The Critical Difference
The terms "bulging disc" and "herniated disc" are often used interchangeably, but they describe two very different situations. The key distinction lies in the integrity of that tough outer wall, the annulus fibrosus.
What is a Disc Bulge? The "Over-Stuffed Hamburger" Analogy
A disc bulge is a condition where the disc sags and extends, or "balloons," outward from its normal space between the vertebrae. The most important thing to know about a bulge is that the outer wall (the annulus fibrosus) remains intact. There is no tear or rupture.
Radiologists, the specialists who read your MRI, define a bulge as a broad-based outpouching that involves more than a quarter (25%) of the disc's total circumference. This is why some experts use the analogy of a "hamburger that's too big for its bun". The entire disc is slightly flattened and sags outward evenly.
Disc bulges are extremely common and are often a normal part of the aging process, known as degenerative disc disease. As we age, our discs naturally lose water content and become less flexible. As the disc flattens, the annulus can lose tension and bulge outward, much like a car tire that has lost some air. In many cases, a bulging disc causes no symptoms at all.
What is a Disc Herniation? When the "Jelly" Escapes
A disc herniation is a more specific and often more significant event. Unlike a bulge, a herniation is defined by a tear or rupture in the annulus fibrosus. This tear creates a weak spot, allowing the soft, gel-like nucleus to push through the wall and leak out into the spinal canal.
This is why a herniation is often called a "ruptured disc." The term "slipped disc" is also commonly used, but it's a misnomer—the entire disc doesn't actually slip out of place. Radiologically, a herniation is a focal event, meaning it affects less than 25% of the disc's circumference.
A Deeper Look: Protrusion, Extrusion, and Sequestration
Your MRI report might use even more specific terms to classify the type of herniation. Understanding these can give you a clearer picture of what the radiologist observed:
- Protrusion: This is the mildest form of herniation. The "jelly" pushes through a tear in the inner layers of the annulus, but the outermost layers are still holding it in. The base of the herniated material is wider than the part that is sticking out.
- Extrusion: This indicates a more complete tear. The nucleus material has burst through the outer wall entirely. The displaced material is wider than the base connecting it to the disc, often looking like a mushroom. The "jelly" is now officially outside the "donut".
- Sequestration: This is the most advanced
stage. A piece of the extruded nucleus material breaks off completely from the disc and
becomes a "free fragment" floating in the spinal canal. This fragment can move, potentially
irritating nerve roots at different locations.
The Hidden Cause of Pain Your MRI Misses: Chemical Inflammation
Here is a crucial point that is often overlooked: the severity of your pain is not always related to
the size of the herniation. A large disc bulge might cause no pain, while a tiny herniation can be
excruciating. Why?
The answer lies in biochemistry. While a bulge can cause pain by physically pressing on a nerve, a herniation adds a second, powerful pain-causing mechanism: chemical irritation. The material of the nucleus pulposus is recognized by your body's immune system as a highly inflammatory substance. When it leaks out and comes into direct contact with a nerve root, it triggers a severe inflammatory response. This chemical fire is a primary driver of the intense, burning, and radiating nerve pain known as sciatica. This is why treating the inflammation is just as important as addressing the mechanical pressure.
Reading Your MRI Report: What Are the Doctors at Germanten Looking For?
An MRI (Magnetic Resonance Imaging) scan is the gold standard for diagnosing issues with the soft tissues of your spine, like discs and nerves. Unlike an X-ray, which is excellent for looking at bones, an MRI provides a crystal-clear, detailed view of the discs, spinal cord, and nerve roots.
When one of our spine specialists at Germanten Hospitals reviews your MRI, they are performing a
systematic evaluation—a meticulous process of digital detective work. They aren't just looking for
one thing; they are assessing the entire ecosystem of your spine.
A Specialist's Checklist for Your Spine
Here's what our experts are trained to look for:
- Location and Severity: The first step is to pinpoint the exact location of the problem (for example, the L4-L5 and L5-S1 levels in the lower back are the most common sites for herniations). We then characterize the finding: Is it a broad bulge or a focal herniation? If it's a herniation, is it a protrusion, extrusion, or sequestration? The size and type are carefully noted.
- Nerve Compression (Impingement): This is perhaps the most critical part of the analysis. Is the displaced disc material physically touching or compressing a nerve root or the spinal cord?. This direct impingement is the classic cause of radiculopathy (sciatica), which leads to pain, numbness, or weakness that travels down an arm or leg.
- Spinal Stenosis: We evaluate the overall space available for your nerves in the spinal canal. A large herniation, often combined with other age-related changes like thickened ligaments or bone spurs, can cause a narrowing of this canal. This condition, called spinal stenosis, can cause pain or heaviness in the legs, especially with walking.
- Overall Disc Health: The MRI gives us a clear picture of the general condition of your discs. A healthy, well-hydrated disc appears bright on certain MRI images. A degenerated, dehydrated disc will look darker and may have lost height. This tells us about the underlying process of degenerative disc disease that may be contributing to the problem.
- Annular Tears: Sometimes, the MRI can
visualize small tears in the annulus fibrosus even without a full herniation. These tears
can be a significant source of localized back
pain, as inflammatory substances can leak through and irritate nearby
nerve endings.
The Most Important Thing Your Doctor Might Not Tell You About Your MRI
Now we come to the single most important piece of information for any patient reading their MRI
report. This is a fact that can instantly reframe your perspective and alleviate a tremendous amount
of anxiety.
Why Your MRI Report Doesn't Tell the Whole Story
An MRI is a picture. It is an incredibly detailed and valuable picture, but it is not a diagnosis.
Decades of high-quality research have shown, without a doubt, that "abnormal" findings on spinal
MRIs are incredibly common in people who have absolutely no pain.
Many of the findings that sound so alarming on a report—disc degeneration, disc bulges, even disc
protrusions—are often just normal, age-related changes. They are the spinal equivalent of getting
wrinkles on your skin or grey hairs. They are a sign of time passing, not necessarily a sign of a
disease that needs fixing.
A landmark systematic review and meta-analysis published in the American Journal of Neuroradiology in 2015 compiled data from over 3,100 pain-free individuals to see what their spines looked like on an MRI. The results are eye-opening and provide powerful, reassuring context.
(Data synthesized from Brinjikji et al., AJNR, 2015)
Let this data sink in. If you are 40 years old and your report says you have a "disc bulge," you are
in the same boat as half of all other 40-year-olds walking around with no pain
at all. If you are 60 and your report mentions "disc degeneration," you share that trait with nearly
90% of your pain-free peers.
This doesn't mean your pain isn't real. It absolutely is. What it means is that the finding on the
MRI might just be an incidental finding—something that has been there for years without
causing a problem, and not the true source of your current pain.
So, What Really Matters? The Power of Clinical Correlation
This brings us to the heart of expert spine care. If the MRI picture alone can be misleading, what
truly determines your diagnosis? The answer is clinical
correlation.
"We Treat Patients, Not Pictures" - The Germanten Philosophy
At Germanten Hospitals, this is our guiding principle. An MRI report is just one tool in our diagnostic toolkit. The most important information comes from you. A diagnosis is only made when we can perfectly match the findings on your MRI scan to the specific symptoms you are experiencing.
This process of clinical correlation is a meticulous investigation that involves:
- A Detailed Medical History: We listen carefully to your story. When did the pain start? What does it feel like? Where does it travel? What activities make it better or worse?.
- A Thorough Physical Exam: We assess your range of motion, flexibility, and look for areas of tenderness.
- A Precise Neurological Exam: We test your
muscle strength, reflexes, and sensation to see if there are any deficits. We may perform
specific maneuvers, like the straight leg raise test, which can help us identify nerve
irritation.
An expert spine specialist's job is to connect the dots. For example, if your MRI shows a herniation
at the L5-S1 level compressing the S1 nerve root on the right side, do your symptoms match? Do you
have pain radiating down the back of your right leg to your foot, and weakness when you try to stand
on your tiptoes? If the picture on the scan and the story your body is telling don't align, then the
finding on the MRI is likely not the culprit. This is how we identify the true "pain generator" and
avoid unnecessary treatments or surgeries.
Your Path to Recovery: From Conservative Care to Advanced Solutions
Understanding your diagnosis is the first step. The next is understanding your path to recovery. And
here, there is more good news.
The Good News: Most Disc Issues Heal on Their Own
The natural history of most disc-related pain is overwhelmingly positive. The vast majority of patients—up to 90% in some studies—with a new disc herniation and sciatica will get significantly better on their own with conservative, non-surgical care.
Your body has a remarkable ability to heal. Over time, the inflammatory response subsides, and the
body can even reabsorb the herniated disc material, causing it to shrink and pull pressure off the
nerve. This process typically takes about 4 to 6 weeks for symptoms to improve significantly, though
full resolution can take a few months.
Conservative Treatment Options: Your First Line of Defence
The goal of initial treatment is to manage the pain and inflammation while your body does its natural healing work. This typically includes:
- Activity Modification: Short periods of rest can help, but prolonged bed rest is not recommended as it can lead to stiffness and muscle weakness. Gentle activity, like walking, is encouraged.
- Physical Therapy: A skilled physical therapist can guide you through specific exercises to strengthen your core muscles, improve flexibility, and teach you proper posture and body mechanics to protect your spine.
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and the chemical irritation of the nerve root. Muscle relaxants may also be prescribed.
- Spinal Injections: An epidural steroid
injection can be a very effective tool. Under X-ray guidance, a potent anti-inflammatory
medication is delivered directly to the site of the nerve irritation, providing powerful
pain relief that can create a window of opportunity for physical therapy to be more
effective.
When is Surgery Necessary? Understanding the "Red Flags"
Surgery is only considered when conservative treatments have failed to provide relief, or in the presence of specific "red flag" symptoms. These are signs of severe nerve compression that require urgent attention:
- Progressive Neurological Deficit: Significant and worsening weakness in your leg or arm.
- Cauda Equina Syndrome: This is a rare but serious medical emergency caused by severe compression of the nerve roots at the end of the spinal cord. Symptoms include loss of bowel or bladder control, and numbness in the "saddle" area (genitals and rectum). If you experience these symptoms, you should seek emergency medical care immediately.
- Intolerable Pain: Pain that is so severe
it cannot be controlled with medication and significantly impairs your quality of life, and
has not improved after an adequate trial (usually at least 6 weeks) of conservative
care.
The Germanten Advantage: Precision Spine Care When It Matters Most
If surgery does become the right path for you, this is where the unique strengths of Germanten
Hospitals truly shine. Our entire approach is built on the principle of precision—using the most
advanced technology to solve the specific, confirmed problem with the least possible impact on your
body.
Harnessing German Technology: Minimally Invasive and Robotic Spine Surgery
Long gone are the days of large incisions and lengthy, painful recoveries. Modern spine surgery is a story of micro-technology and precision engineering.
- Minimally Invasive Spine Surgery (MISS): Using techniques like Endoscopic Discectomy, our surgeons can remove a herniated disc through an incision that is often less than a centimeter long. Working through a small tube with a high-definition camera, we can gently move muscle tissue aside instead of cutting it. For our patients, this means significantly less pain, a lower risk of infection, and a dramatically faster recovery—many patients go home the same day.
- Robotic-Assisted Spine Surgery: For more
complex procedures that require stabilization, we utilize the latest in robotic guidance
systems. This technology allows our surgeons to plan the procedure in a 3D virtual space and
then execute that plan with sub-millimeter accuracy. Studies have shown that robotic
assistance allows for screw placement with over 98% accuracy, enhancing safety, reducing
operating time, and minimizing radiation exposure for both the patient and the surgical
team.
This combination of minimally invasive techniques and robotic precision ensures that we are targeting
only the source of the problem, preserving healthy tissue, and getting you back to your life faster
and more safely than ever before.
Your Next Step: Taking Control of Your Spinal Health
Your MRI report is a starting point, not a final destination. It is a valuable piece of data, but it
does not define you or your future. The most important takeaway is this: do not panic. The path to
recovery begins with a clear understanding of the true source of your pain, and that can only be
achieved through a comprehensive evaluation by a spine expert who knows how to connect the dots
between your imaging, your history, and your physical symptoms.
At Germanten Hospitals, our
world-class team, led by pioneers like Dr. Mir Jawad Zar
Khan, is dedicated to providing precisely that. We combine deep clinical
expertise with the most advanced diagnostic and surgical technologies to offer a level of care that
is both sophisticated and deeply personal.
Don't let an MRI report dictate your life. Let us help you decode it.
Schedule a comprehensive evaluation with the spine specialists at Germanten
Hospitals today. Let our experts provide the clarity you deserve and
create a personalized treatment plan to guide you back to a pain-free, active
life.
Frequently Asked Questions (FAQs)
Q: Can a bulging disc heal on its own?
The symptoms from a bulging disc often resolve on their own over 6-8 weeks with conservative care.
While the bulge itself may not disappear, the pain and inflammation can subside, allowing you to
live symptom-free.
Q: Is a "bulging disc" the same as a "slipped disc"?
No. "Slipped disc" is
a common but inaccurate term for a disc herniation, where the inner material has actually ruptured
through the outer wall. A bulge is a less severe condition where the outer wall remains intact.
Q: How long does a herniated disc take to heal without surgery?
Most
patients feel significant improvement within 4 to 6 weeks. However, it can sometimes take several
months for the body to fully reabsorb the herniated material and for all symptoms to
resolve.
Q: What is the best sleeping position for a herniated disc?
Many people
find sleeping in the fetal position (on your side with your knees drawn up towards your chest) to be
the most comfortable, as it can open up the spaces between your vertebrae and relieve pressure on
the nerves. Placing a pillow between your knees can also help keep your spine aligned.
Q: How bad does my herniated disc have to be to need surgery?
The decision
for surgery is based less on the size of the herniation and more on your symptoms. Surgery is
typically considered only when you have persistent, debilitating pain that hasn't improved with
conservative care, or if you develop progressive neurological symptoms like significant weakness or
loss of bowel/bladder control.
Q: What is the success rate of microdiscectomy surgery?
For relieving
radicular pain (the pain that shoots down your leg or arm), microdiscectomy is a highly successful
procedure. Studies consistently show success rates in the range of 80-90% for significant pain
relief.